
Are you looking for information about weight loss surgery? Dr Crawford has a website full of information including the cost of bariatric surgery, videos and more.
Obesity Surgery
For detailed information including cost of bariatric surgery, please visit Dr Crawford’s Obesity surgery website.
Introduction
The fact that you are reading this means that either you or someone you know is considering the life-altering decision to undergo weight loss surgery. This is an important decision, and should not be made without considering all the facts.
This booklet has been designed to help you understand the following:
- The health problems associated with obesity
- Advantages and disadvantages of weight loss surgery
- Descriptions of the surgical procedure
- Risks associated with weight loss surgery
- The next steps to take
Please bear in mind that the information provided here is not a substitute for the opinion and advice of a qualified doctor or surgeon. Your best source of information is an experienced surgeon.
The Team
We are dedicated to providing multidisciplinary expert management of your weight problem. The team includes a specialist surgeon, an assistant surgeon, a nutritionist, and others, dedicated to treatment of and research into obesity related health problems, and of course our friendly office staff.
We are located at the Royal Prince Alfred Hospital Medical Centre in Newtown and The Mater Clinic in North Sydney. The surgery is performed at the Mater Hospital in North Sydney, backed by a great team of nurses and clinicians.
Am I a Candidate for Weight Loss Surgery?
Obesity is becoming an increasingly prominent health problem in our society. Approximately 15% of men and women in Australia are obese, with 4-6% classified as morbidly obese. This number is increasing. Obesity is associated with a number of health problems and importantly is associated with a reduced life expectancy. Body Mass Index (BMI) is a method for measuring obesity and relates to a person's height and weight. A BMI score is derived by dividing a person's weight (in kilograms) by their height (in metres) squared. BMI=wt/(ht x ht)
For example, a person who is 183cm tall and weighs 95kg will have a BMI of 28.4
ie. 95 divided by (1.83 x 1.83). The severity of obesity is defined using the following table of BMI scores:
| BMI | |
| Normal | 20-25 |
| Overweight | 25-30 |
| Obese | 30-35 |
| Severely Obese | 35-40 |
| Morbidly Obese | 40-50 |
| Super Obese | 50+ |
Associated health risks
There are a number of medical conditions that have a direct association with obesity. These include type 2 diabetes, hypertension, fatty liver disease, respiratory problems, female infertility, and psychological problems such as depression. Patients who are obese are more likely to suffer from coronary heart disease and stroke. There is clear evidence that obesity is associated with reduced life expectancy. Those who are morbidly, or super obese face a risk of dying that is twice that of others of the same age.
In addition to the diseases mentioned above, obesity has a number of immeasurable negative effects. Morbidly obese people often have a low sense of self-esteem and it is common for them to suffer from depression and to withdraw from social interactions at many levels.
Dieting
Those people who are able to maintain a healthy low calorie diet will be able to lose weight and maintain a normal BMI in the long term. Unfortunately for the majority of people who have become obese, dieting will only produce transient, temporary weight loss.
Randomised controlled trials have shown that surgery results in greater weight loss than diets. This weight loss is maintained over a longer period when compared with even the best of diets.
Importantly, studies have shown that mortality (risk of dying) is significantly reduced in patients who undergo surgery for weight loss when compared with those who don’t.
Why Surgery?
Weight loss surgery should be considered if you:
- Are unable to achieve a healthy body weight for a sustained period of time, even through medically supervised dieting and exercise.
- Have a Body Mass Index (BMI) of over 40
- Have a BMI of over 35 and are experiencing negative health effects
- Weigh more than 45 kg above your ideal body weight
- Are highly motivated and committed to long term lifestyle changes
Where to Begin?
This information booklet has been designed to give you a better understanding of the risks and benefits of weight loss surgery. In the end though, your best source of information is an experienced laparoscopic surgeon who knows how to handle your special needs before, during and after weight loss surgery.
Choosing Surgery
If your goals are to live better, healthier and longer, you may want to choose weight loss surgery to help you achieve your goals. Weight loss surgery is major surgery. That is why you should make the decision to have obesity surgery only after careful consideration and consultation with an experienced surgeon or a knowledgeable family doctor. Your surgeon will be able to answer your questions and explain the exact details of the procedure and the follow-up care required. You will also meet with a nutritionist to explain the dietary expectations after the surgery.
The Importance of Support
The changes in your diet and lifestyle after obesity surgery can last a lifetime. And you'll have a greater chance of long-term success if you surround yourself with people who understand and support your goals. There are things you can do, such as :
- Help your friends and family members understand why you've chosen a surgical weight loss solution.
Discuss your reasons for having surgery; you will be counting on them to help you during and after weight loss surgery.
Weight Loss Surgery
Surgery for obesity has been carried out for over 50 years and numerous advances have been made during this time. In the past, surgery for weight loss was associated with high risks of side effects and complications. Advanced laparoscopic (keyhole) techniques have allowed this to become a safe and reliable means of achieving and maintaining weight loss.
Surgical treatment of obesity is a major undertaking. It necessitates undergoing major surgery and requires a lifelong commitment to compliance with post- operative medical care. It is not a cosmetic procedure for those who are unhappy with their body image, but rather a medically proven treatment for an established health problem. Generally, gastric band surgery has proven benefits for those with a BMI >40, or those with a BMI over 35 with established obesity related health conditions. Patients should have seriously attempted to achieve and maintain weight loss before considering surgery.
Types of surgical procedures
Bariatric surgeons first began to recognise the potential for surgical weight loss while performing operations that required the removal of large segments of a patient's stomach and intestine. After the surgery, doctors noticed that in many cases patients were unable to maintain their pre-surgical weight. With further study, bariatric surgeons were able to recommend similar modifications that could be safely used to produce weight loss in morbidly obese patients. Over the last two decades these procedures have been continually refined in order to improve results and minimize risks. Today's bariatric surgeons have access to a substantial body of clinical data to help them determine which weight loss surgery should be used and why. Today, there are two basic approaches that weight loss surgery takes to achieve change:
- Restrictive procedures that decrease food intake. This includes sleeve gastrectomy (and gastric banding).
- Malabsorptive procedures that alter digestion, thus causing the food to be poorly digested and incompletely absorbed so that it is eliminated in the stool. This can also incorporate an element of restriction. Gastric bypass is an example of this type of procedure.
Sleeve Gastrectomy: Not only limits how much can be eaten at one time, but also decreases hunger between meals by pressure in the upper stomach and removal of the part of the stomach responsible for the ‘appetite hormone’ (ghrelin).
Gastric Banding?
The surgical placement of a soft band around the uppermost part of the stomach. This is performed using laparoscopic (keyhole) surgery, which involves several small holes in the abdomen, rather than a single large incision. Gastric banding was the most commonly performed weight loss surgery in Australia for a decade, but has been gradually replaced by sleeve gastrectomy.
Dr Crawford no longer performs gastric banding because the long term results of this prosthesis are disappointing with respect to slippage, erosion and re-operation.
What is Sleeve Gastrectomy?
Sleeve Gastrectomy is performed using laparoscopic (keyhole) techniques to resect and remove a large segment of the stomach (up to 80% of the total volume), whilst maintaining the normal passage of food anatomically. The remaining stomach looks very similar to a normal stomach, only much narrower. The capacity of the stomach is reduced from about 1.5 litres of food and liquid to approximately 300mls, and this provides the brain feedback via stretch receptors that signal that feeling of fullness and satiety. Severe hunger is reduced. Despite being smaller, the remaining stomach will still function normally.

The surgery involves a number of small incisions in the abdomen, and dissection and stapling off of the excess stomach (which is removed from the body), using special stapling devices. The new edge of the stomach is then reinforced with a suture to minimize the risk of leak.
Prior to Surgery
You will need to be on an ‘Ultra-low Calorie Diet’ before surgery. Optifast is taken for 2 weeks to replace ALL meals. If you feel you MUST have something else, then it needs to contain very few calories. (Salad or steamed vegetables without dressings or oil for a ‘treat’). Check with the nutritionist.
The usual stay in hospital is 3 post-operative nights.
Following Surgery
Day 2-7: Fluids that could be sucked through a thin straw.
Day 7 to week 3-4: Pureed food.
Week 4+: Slow introduction of some more solid foodstuffs thereafter, as guided by the team.
- Progress from thin to thick only after the thinner fluids are easily tolerated
Reflux/heatburn is occasionally experienced early after sleeve gastrectomy, you will therefore have an anti-acid tablet for 30 days. Sometimes it persists long-term and an anti-acid treatment might be required.
The Steps of a Laparoscopic Sleeve Gastrectomy
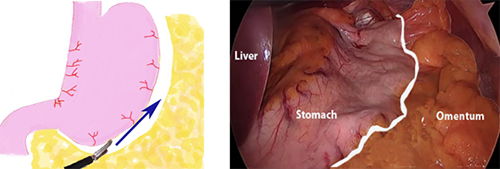
Step 1. The omentum is separated from the greater curve of the stomach.
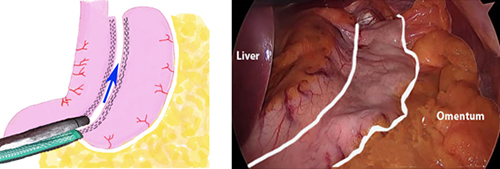
Step 2. The sizing tube is passed through the mouth and the stomach is divided with 6-7 fires of the stapler.
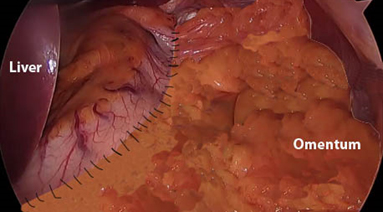
Step 3. The staple line is oversewn, with omentum support.
Comparing Laparoscopic Gastric Band Surgery with Sleeve Gastrectomy
| Laparoscopic Gastric Band | Laparoscopic Sleeve Gastrectomy | |
| Safety | Safest (major complications are rare) | Safe (around 1% major complication rate) |
| Adjustability | Very adjustable | Set once at surgery |
| Success | Successful | More successful |
| Need for more surgery or procedures | High | Low |
| Frequency of doctor appointments | High | Low |
| Restrictions of certain foods | High | Low |
| Reflux | More likely | Less likely |
| Long-term Satisfaction | Good | Better |
| Reversibility | Yes | No |
| Convert to the other procedure later | Yes | No |
| Hospital stay | Overnight | 2-3 nights |
| Return to solid food | 3-4weeks | Up to 6 weeks |
The Sleeve gives a slightly higher long-term weight loss on average, is less fuss and less restrictive in food choices. It is slightly more dangerous surgery up front, but thereafter is probably more comfortable for patients and there is less need for follow-up appointments.
General Advice and Possible Minor Side-effects after Sleeve Gastrectomy
Vomiting
Patients may vomit or feel pain after food intake. This can be can be caused by swallowing too quickly, trapping air, or un-chewed chunks of food getting stuck. By eating slowly and calmly, you will learn to listen to the signals from your stomach. Notify Dr Crawford if new or persisting vomiting develops after you are home.
Vitamins
During the phase of rapid weight reduction, vitamin supplements are advisable. A chewable or liquid vitamin mixture containing multivitamins, in particular the vitamin B complex, is recommended following surgery. Your nutritionist will give you advice around vitamens.
Pregnancy
The period between surgery and weight stabilisation is considered to be a period of starvation. It is not advisable to become pregnant during starvation, despite the fact that the foetus has priority over the mother with regard to food. Should you nevertheless get pregnant, it is advisable to let Dr Crawford and your nutritionist know. You should wait until your weight has stabilised before becoming pregnant.
Medication
Tablets must be broken down into small pieces or crushed before they are taken. It is common that medication for conditions such as hypertension, diabetes or asthma may need to be altered (reduced) after this operation. Patients should consult their doctor about this.
Doctor Appointments
After surgery you must undergo regular check-ups as an outpatient. Initially, these check-ups will be carried out often, but soon visits will yearly if everything is going ok.
Physical Activity
It will be important to alter not only your eating habits, but also your level of physical activity. You should to start exercising slowly after surgery. As weight loss is achieved, physical activities will gradually become easier.
Take this information booklet with you to talk to your local doctor about laparoscopic sleeve gastrectomy
It can be very helpful for you to discuss the procedure with your General Physician. Take this information with you so that your GP can help explain parts to you or to jog your memory.
You should plan to visit your GP yearly after surgery for a check-up and blood test.Long term follow-up and lifestyle
In order to get the best results from your surgery, it is important that you are committed to long term changes. Regular consultations may be necessary to review your progress, monitor your weight and health, advise you on diet and exercise and look for any long term problems.
Your commitment to dietary and lifestyle changes is essential to ensure the success of your surgery. In the long term you should eat small healthy meals and drink only liquids containing little or no calories such as water, tea, coffee and drinks.
Regular exercise should be a part of your weight loss program and you should aim to exercise for at least 20 to 30 minutes every day.
The next steps
Questions for My Surgeon
Here are some of the questions you should ask your surgeon:/
- Can this surgery be performed using minimally invasive techniques?
- Can I be considered a candidate for surgery?
- Which weight loss procedure is best for me? Why? What are the risks involved?
- What is the length of my anticipated hospital stay?
- How will my eating habits change?
- Do you have information about obesity surgery costs and payment options?
- What is the typical weight loss and improvement of health conditions?
Potential complications of sleeve gastrectomy
Thankfully serious/major complications are rare, but nonetheless they could occur.
- Leak This is the complication that worries bariatric surgeons the most with respect to this procedure. The leak is caused by a combination of the intentionally high pressure remnant stomach and either a failure of staples or a failure of healing. Most leaks occur in the upper part of the staple line where the healing can be most compromised.
Leaks could occur
- early (within days of surgery) while you are still in hospital, with peritonitis. You would need another keyhole surgery to washout and drain the infected fluids, and other procedures such as stents until it healed.
- later (within weeks of surgery) when you are home recovering. The symptoms are sometimes subtle but include new vomit, cough, fever or sweats. These leaks would usually cause an abscess (localized collection of pus) around the upper stomach. These are usually managed with small plastic tubes (stents) placed by an endoscope.
- Previous surgery (particularly gastric band) due to the scar tissue build up and the possibility of folded over stomach in the staple line. This is thought to be particularly when the removal of band is performed at the same time as the sleeve operation.
- Too tight sleeve. We know that as we tighten the remaining stomach by using smaller sizing tubes, we run into more problems from leak because of pressure.
- Other technical aspects, such as type and size of staples, the use of buttressing, the presence of a sliding Hiatus Hernia, where the upper stapleline could be ‘sucked’ up into the negative pressure of the chest influence leak rates.
- Preventing a leak The best method for preventing a leak is to employ all of the techniques that we know can minimize it. It is Dr Crawford’s practice to:
- Separate the removal of the band from the sleeve gastrectomy surgery by at least 3 months to allow for scar tissue to soften
- Use ‘Seam-Guard’ buttressing for the final two staple loads.
- Oversew the entire staple line, with omental re-inforcement.
- The risk of a leak: The overall risk of a leak is between 1-2%. Dr Crawford will explain if he thinks your risk is higher than this.
Other Potential Complications
These include but are not limited to the following which are similar for almost any abdominal surgery.
- Wound infection
- Bleeding
- Clots
- Pneumonia
- Heart trouble
- Hernia
- Bowel obstruction
Frequently Asked Questions
Won’t I feel hungry all the time if I am eating less
No, the Sleeve Gastrectomy takes away the strong hunger urges between meals. If you are feeling hungry, then see the nutritionist or Dr Crawford for advice.
Will I need to be on a special calorie controlled diet?
No, the sleeve works by restricting how much you eat rather than how many calories you take. Obviously for the best results you should try to eat as healthily as possible, and your nutritionist will be able to advise you more on this.
How long will I need off work?
This varies for different people. The in hospital recovery is quick with most people going home a day or two after surgery. The average time off work is 2 weeks.
Will the procedure be able to be reversed if I am unhappy with it?
No, a Sleeve Gastrectomy is a permanent change. Satisfaction levels are usually very high.
How will I be able to go out for a meal if I am restricted in intake?
This does worry some people, but we will give you advice about ways of dealing with this. You can still enjoy a meal with friends or family even if you are eating less.
Are there any types of food I won’t be able to eat?
There may be some foods that are particularly challenging. These are usually those that require a lot of chewing. Most find they can eat all normal food with a little extra chewing (just a lot less of it).
Contact Us
This information is intended as a guide only. Please bear in mind that the information provided here is not a substitute for the opinion and advice of your surgeon. Your best source of information is an experienced surgeon who specialises in the management or control of obesity.
You will need a referral from your local doctor.
Please call (02) 9565 4854 for an appointment with Dr Michael Crawford.
Dr Crawford sees patients at:
Suite 314, RPAH Medical Centre 100 Carillon Avenue, Newtown
Or
The Mater Clinic,198 Pacific Hwy, North Sydney
Watch a video "Sleeve Gastrectomy explained with Dr Michael Crawford" at my website or on youtube: www.youtu.be/pv7f77sWT4A
| Gastric Band Surgery. Dr Crawford no longer performs this surgery | 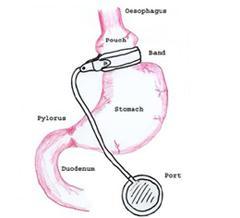 |
 |
Sleeve Gastrectomy A large portion of the stomach is removed using a stapling device that seals the stomach as it cuts through. A narrower, tube shaped stomach is formed. |
![]() Bariatric / Obesity Surgery – Patient Information
Bariatric / Obesity Surgery – Patient Information
You will need the Adobe Reader to view and print these documents. ![]()





 Meet
Meet



