Liver Cancer
Information for Patients
Liver Cancer is classified into Primaries and Secondaries.
Primary Liver Cancer.
Primary Liver cancer is where the cancer arises from the cells within the liver. There are two main types, and a few other very rare types.
Hepatocellular Carcinoma :: Cholangiocarcinoma
Hepatocellular Carcinoma
Also known as hepatoma or HCC. This is the most common primary liver cancer. It arises from the main liver cells known as hepatocytes.
Predisposing factors
HCC is most commonly (90%) associated with chronic liver disease. Cirrhosis of the liver is usually present by the time a cancer grows. In these circumstances the cancer has grown as a result of repeated inflammation and repair within the liver.
The other 10% of HCC grow spontaneously or as a result of transformation from an adenoma (a benign growth). Some of these are called fibro-lamellar HCC because of their appearance.
HCC tends to start off growing quite slowly and as it gets bigger it gets more aggressive and can spread.
Diagnosis
HCC is most commonly diagnosed in this country by a screening test performed on someone with cirrhosis. Often this will be a blood test (alpha-feto-protein) which becomes elevated in around 60% of patients with HCC. Other tests to detect HCC are Ultrasound and CT scans of the liver.
Once a tumour is identified, further tests are performed to determine the best treatment option. These tests may include CT scans, MRI scan, angiograms, portal venous wedge pressures, and biopsy of the non-cancerous liver (to check for cirrhosis).
Biopsy of the liver tumour is rarely required and may cause bleeding or spread of the cancer. Biopsy of the tumour should only be performed if the cancer is felt to be incurable by either liver resection or transplant.
Prognosis
The prognosis (expected outcome) with HCC varies greatly according to the size and number of the cancers, whether there has been any invasion into veins, and whether there has been any spread. The prognosis is also affected by the degree, if any, of cirrhosis.
Treatment

- Surgery (Liver Resection). The best treatment for HCC is the complete removal of the tumour. This is only possible in around 15% of those found to have HCC because; the tumour has already spread, or is in a vital area of the liver that can’t be removed, or because the cirrhosis is so advanced that surgery is too dangerous. Liver resection will cure up to 40% of patients operated on, with much of the recurrence after surgery being the growth of new cancers in a diseased liver.
- Liver Transplant. Liver transplant is suitable for some patients with small HCCs where the cirrhosis makes it too dangerous to remove the tumour with resection. Liver transplant can cure up to 70% of highly selected patients.
- Local Ablation. There are numerous techniques now available to kill off small HCCs without removing them. These include Radio-Frequency-Ablation (RFA), Cryotherapy, Alcohol or Ascetic Acid injection. These treatments are all limited to the treatment of relatively small HCCs (generally <4cm diameter).
- Trans-Arterial Chemo-Embolisation (TACE). Chemotherapy as a pill or in a vein is not very effective against HCC. However, high dose chemotherapy delivered directly to a cancer via the artery to the liver can be effective at shrinking HCC, and is frequently used for larger tumours.
- Iodine131 Lipiodol. This is a radioactive substance that can be injected into the artery supplying the liver and ‘homes in’ on HCC to deliver a concentrated radiotherapy effect while sparing the remainder of the liver. It has effects similar to TACE.
Cholangiocarcinoma
Cholangiocarcinoma is the other main liver cancer primary and is a tumour of the bile ducts cells. It can occur near the main ducts just beyond the liver or deep in the liver itself.
Predisposing factors
Patients suffering with chronic inflammatory conditions of the bile ducts such as the rare disorder of Primary Schlerosing Cholangitis, are at a higher risk of developing cholangiocarcinoma. Oftentimes, however, there is no clear predisposing factor evident, although, like nearly all cancers, advancing age is often present.
Diagnosis
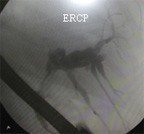
Cholangiocarcinoma may present as either a lump seen on CT scan or because it has caused blockage of the bile duct leading to jaundice (yellow colouring). Weight loss, poor appetite and nausea may be present. Investigations to confirm the diagnosis include CT scans, Ultrasound, MRI scans, Endoscopic Retrograde Cholangio-Pancreatography (ERCP), and blood tests.
A needle biopsy is not usually required and may cause spread of the tumour.
Prognosis
The prognosis (expected outcome) with cholangiocarcinoma varies greatly according to the size and position of the cancer, whether there has been any invasion into veins, and whether there has been any spread. The prognosis is also affected by the state of the liver; the degree if any of cirrhosis.
Treatment
- Surgery (Liver Resection). The best treatment for cholangiocarcinoma is the complete removal of the tumour. The ability to remove it depends on the presence of spread and the position of the tumour. It is often necessary to remove a large part of the liver if the tumour arises at the point where the left and right bile ducts merge (Klatskin) tumour. Surgery to resect these tumours can be challenging and sometimes impossible.
- Chemotherapy. Some patients are suitable for chemotherapy, although chemotherapy alone would not be expected to cure this cancer.
- Radiotherapy. External beam radiotherapy can help to shrink tumours that are causing symptoms, but is not curative in this cancer.
- Stenting. For cancers that are blocking the bile duct, and causing jaundice, plastic or metal tubes are often inserted to allow the flow of bile and to relieve the jaundice.
Secondary Liver Cancer
Secondary (Metastatic) liver cancer is where the cancer started elsewhere in the body and spread to the liver. The liver is a very common spot for secondaries to occur. Only liver secondaries that are suitable for surgery are discussed here. Just about any cancer can spread to the liver in late stages.
Colorectal Metastases
The most common treatable liver secondaries are from the rectum or colon (the large bowel). The blood from the bowel runs via the mesenteric and portal veins into the liver, so it is no surprise that the liver is a common site of secondaries from bowel cancer.
Up to 70% of patients with colon or rectal cancer will develop liver secondaries. Around 1/3 of these will have their secondaries confined to the liver, and around 1/3 of those will have removable cancers (resectable disease).
Diagnosis
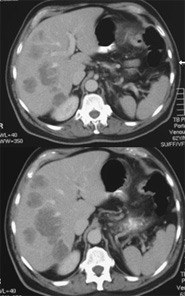
Metastatic Colorectal Cancer in the liver might be present at the time of bowel surgery, or show up months or years later. It might be diagnosed during the original surgery or be found using screening tests following successful bowel surgery. Occasionally the liver secondary is diagnosed before the bowel tumour is apparent. The common screening tests used are a blood test (CEA), and ultrasound or CT scans. Once a liver metastasis has been found it is crucial to work out whether it is alone or there are others. If there are others it is important to know whether they are only in the liver or whether there is cancer elsewhere. To help work this out patients have CT scans, chest x-ray, blood tests and a PET scan.
The PET (Positron Emission Tomography) scan is a nuclear scan that relies on an injection of radioactive sugar. Since cancers rely on sugar for their energy and use it more rapidly than normal tissues, the radioactivity accumulates in the cancers, and shows up as a ‘hot spot’ on the scan. The PET scan can diagnose tumours as small as 1cm. Recent evidence shows that patients who undergo liver surgery for colorectal secondaries, who have otherwise negative PET scans, do very well.
Biopsy of the tumour is rarely required and should not be performed if the tumour is resectable.
Prognosis
The prognosis (expected outcome) with colorectal cancer metastases varies according to resectability. For patients with removable tumours, the long-term (5 year) survival is around 40%. For those with widespread disease, long-term survival is limited, but chemotherapy when suitable is likely to prolong life.
Patients with metastatic colorectal cancer are best looked after with a multi-disciplinary team approach that includes specialist surgeons, oncologists and nurses.
Treatment
- Surgery (Liver Resection). The best treatment for liver secondaries due to colorectal cancer is the complete removal of the tumour(s). The ability to remove the tumours depends on their position, number and whether there is spread outside the liver. Up to 70% of the liver can be removed to clear the cancer.
- Chemotherapy. Some patients are suitable for chemotherapy, although chemotherapy alone will not cure colorectal metastases. Chemotherapy has a role in shrinking tumours and extending life. There is emerging data about surgery following (Neo-Adjuvant) chemotherapy, where the chemotherapy has shrunk a previously un-resectable tumour down to a resectable one. (Adjuvant) Chemotherapy is usually recommended after successful surgery to ‘mop up’ any small tumour deposits that might be undetected.
- Other treatments. There is thus far little convincing evidence for other treatments for liver secondaries from colorectal cancer.
Non-Colorectal Metastases
Many other tumours spread to the liver. Liver resection is sometimes appropriate for neuroendocrine, renal, melanoma and some sarcomas. Resection for other secondaries is not usually indicated.
![]() Click Here for more information about liver surgery.
Click Here for more information about liver surgery.
You will need the Adobe Reader to view and print these documents. ![]()






 Meet
Meet



